FAQs About In-Center Sleep Studies
An in-center polysomnography (PSG) test takes place at one of our many convenient sleep center locations. These sleep centers offer all the comforts and amenities of home, including a private, comfortable room where you can relax and have a typical night’s sleep.
PSG records your brain waves, heart rate and breathing as you sleep. It also charts your eye movements, limb movements and oxygen in your blood. PSG can diagnose or rule out sleep disorders such as obstructive and central sleep apnea, restless leg syndrome (RLS) and more in adults and children.
In children, PSG may be used to diagnose or rule out suspected sleep apnea due to enlarged tonsils or adenoids; an obese child may have OSA due to excess fat around the airway.
A titration is a test that is used to determine your optimal positive airways pressure (PAP) settings. Proper PAP settings can eliminate most or all apnea events. It is performed when a patient has been previously diagnosed with sleep apnea through one of our sleep studies (either in-center or in-home) and have been placed on PAP the entire night.
Learn more about the types of studies we perform in our sleep centers.
If your doctor refers you to us for a sleep study, you can expect to be contacted by our customer service team once we have processed your referral and have all of the appropriate information (insurance details, contact information and progress notes).
You can also contact us directly by calling (877) 775-3377 Monday through Friday 8am to 6pm.
Most sleep studies start in the evening. Most of our appointments start between 9pm and 10:30pm. There may be multiple patients scheduled per each technician at the sleep center. The technician will spend around 45 minutes with each patient completing the hook-up where electrodes are placed on the patient’s head, face and body.
Depending on the number of patients and the start time of the appointment, most PSGs will end at about 5:30am to 6:00am the following morning.
Two-piece pajamas (separate top & bottom). Undergarments do not qualify as pajamas (such as men’s boxers) and shorts or sleeping pants must be worn.
Even though you may have a favorite night gown or prefer to sleep au naturel, two-piece pajamas are a must for the comfort of the technician performing your study and the need to attach electrodes and leads in various positions (around your waist and legs, etc.).
Here are some examples of appropriate, two-piece pajamas to wear to a sleep study:

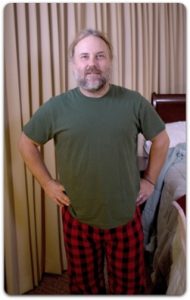
- Pajamas (separate top and bottom)
- Toothbrush and toothpaste
- Book/magazine (to help get you settled to fall asleep or if you have to wait for a few minutes during set-up)
- Health insurance card, driver’s license or ID, and co-pay/co-insurance
- Snack/water bottle (if you need mid-night snacks or an early feeding bring a snack bar or piece of fruit. There will be water on-site, but it’s nice to have your own on-hand).
- Pre-study questionnaire. You can complete the questionnaires about your insurance and medical history online, or can you fill them out by hand when you arrive at the sleep center, but completing it beforehand will give you more time to settle in and ask your technician questions.
You will receive your results in about two weeks (10 business days). Each sleep study is scored by a technician and then reviewed by a sleep specialist. Please contact your referring physician to discuss your results and next steps.
We fax the results to your physician. If you would like, we can also send a copy of the report to you.
Our goal is to watch you sleep so that we can evaluate you for a sleep disorder. When a patient is unable to fall asleep during the evaluation, it precludes our ability to monitor their sleeping patterns. It is common for some patients to take sleeping pills to help achieve the goals of the study.
Points to consider before taking a sleeping aid before your sleep study:
- Continue to take any prescribed medications that you usually take (unless otherwise instructed by your doctor). If you usually take a medication at night, bring it with you to the sleep center.
- List all medication, prescribed or over-the-counter (including any sleep aids), that you have taken, on your medication list in your intake paperwork.
- We don’t know what effect the sleep aid may have on you, so please arrange for safe transportation home from the sleep center in the morning.
- Generally, sleep aids have little or no effect on the diagnosis’s made from your sleep study data, but the reasons for having the sleep study need to be considered. If you are having the sleep study to evaluate sleep disordered breathing, like obstructive sleep apnea, the sleep aid shouldn’t have any effect on your normal breathing patterns. Sleep aids may change your sleep architecture like reducing the latency to sleep onset, altering the depth of sleep, changing the percentage of time spent in some sleep stages and increasing your total sleep time or sleep efficiency which could impact your diagnosis for other sleep disorders like insomnia.
It’s best to talk to your doctor if you have any concerns. Most importantly, please make sure that you include the sleep aid, if you decide to take it, on your medications list.
We don’t recommend drinking before your sleep study
Alcohol impacts sleep; therefore, it may alter your results. For example, some people only have sleep apnea in REM sleep, so if alcohol were to cause you to miss REM sleep during your sleep study, you may have a false negative result.
If you have mild sleep apnea, it may appear worse.
If you’re coming to the sleep center for a titration study, you may be titrated at a different pressure than is required for a normal night of sleeping.
If you’re a smoker and have scheduled or are considering scheduling a sleep study, you’re probably worried about how you’ll make it through the night. Our technical director, Jonathan Sherrill addresses your concerns in this post.
Can I take a smoke break during my overnight sleep study (PSG)?
No. Even if you’re a really heavy smoker, we can’t allow you to leave the facility to smoke in the middle of your sleep study.
Polysomnography measures multiple signals such as breathing, heart rate, eye movements, and more, via electrodes that are placed on your head, face, around your chest and on your legs (learn more about different types of sleep studies and the disorders they diagnose here). It wouldn’t be feasible for the technician to remove the sensors every time a patient needed a cigarette break. Additionally, since the studies take place at night, the access to the sleep centers is often restricted and secured. Leaving the sleep center and then returning to complete the study at night is not possible.
What if I’m having a daytime MSLT after my overnight study- can I smoke then?
You still can’t smoke during your overnight sleep study, but we would allow you to leave the facility to smoke during breaks between naps (learn more about how MSLT daytime studies are used to diagnose or rule out narcolepsy here).
American Academy of Sleep Medicine guidelines require that you stop smoking at least 30 minutes before the start of your next scheduled nap. You would need to coordinate this with your daytime technician.
However, nicotine can contribute to insomnia and since the MSLT specifically measures the latency to sleep onset (how long does it take you to fall asleep?) it may alter the results.
Can I smoke an electronic cigarette during my sleep study?
No. Electronic cigarettes or vaporizers cannot be used in our facilities at any time. For daytime studies, you would follow the same protocol listed above for regular cigarettes.
There are no restrictions for nicotine patches and gum. Please list all medications on your paperwork when you arrive for your sleep study.
What about marijuana and alcohol?
Neither marijuana nor alcohol are allowed to be consumed in our facility during any of our testing. If a patient consumed alcohol or marijuana ahead of the appointment we wouldn’t refuse the study unless the patient’s behavior was inappropriate.
Again, please list all medications on your paperwork when you arrive for your sleep study.
Additionally, color effects absorption of sensor. So, depending on the color of the nail polish, this can affect the ability of the sensor to accurately measure your blood oxygen. Red nail polish is the worst.
If a patient tests with acrylics or nail polish, it’s possible that the starting oxygen reading (called SaO2 value) will be lower than actual baseline. What we’re looking for in the study is any change from the baseline.
If no signal could be obtained during polysomnography, the study would be canceled due to technical issues in place of continuing the recording and repeating. A sleep study is invalid without oximetry.

